CEN/TS 17500:2021
(Main)Quality of care and support for older persons
Quality of care and support for older persons
The services specified in this document are health and social care services for older persons provided by healthcare and social care personnel. This document
- specifies requirements and recommendations for services provided to the older person at home and in care homes, based on the older person's individual needs and preferences to assist self-determination, participation, and a safe and secure old age.
- specifies requirements and recommendations for systematic approaches regarding the service provider’s ability to produce a good quality of care and support for the older person.
- covers services irrespective of the legal form of ownership and whether the service is publicly or privately funded.
- is applicable to care providers, regardless of structure, organization, ownership, size or type of the care services provided.
- can be used by the service provider at all management levels in the organization to plan, lead, implement, maintain, evaluate and improve the quality of the service.
- can be used by the provider for internal audits or self-assessment and/or external parties for certification/accreditation to assess the provider’s ability to meet the older person´s needs and expectations.
- can be used to provide basic information for procurement and education.
- does not cover standardization of medical devices and clinical guidelines.
Qualität der Pflege und Unterstützung für ältere Menschen
Bei den in diesem Dokument aufgeführten Dienstleistungen handelt es sich um Gesundheits- und Sozialfürsorgedienste für ältere Menschen, die von Gesundheits- und Sozialfürsorgepersonal erbracht werden.
Dieses Dokument:
- beschreibt Anforderungen und Empfehlungen für Pflegeleistungen, die den älteren Personen zu Hause und in Pflegeheimen geboten werden, basierend auf den individuellen Bedürfnissen und Wünschen der älteren Person, um die Selbstbestimmung, die Mitbestimmung und ein sicheres Älterwerden zu unterstützen.
- beschreibt Anforderungen und Empfehlungen für systematische Ansätze hinsichtlich der Fähigkeit des Anbieters, eine gute Qualität der Pflegeleistung und Betreuung für die ältere Person zu gewährleisten.
- behandelt Dienstleistungen unabhängig von der Rechtsform und unabhängig davon, ob die Dienstleistung öffentlich oder privat finanziert wird.
- ist auf Anbieter anwendbar, unabhängig von Struktur, Organisation, Trägerschaft, Größe oder Art der angebotenen Pflegedienste.
- kann vom Anbieter der Pflegeleistung auf allen Management-Ebenen in der Organisation zur Planung, Leitung, Implementierung, Aufrechterhaltung, Beurteilung und Verbesserung der Leistungsqualität verwendet werden.
- verlangt vom Anbieter, den Leistungsinhalt der Organisation in einer Dienstbeschreibung zu erläutern, die z. B. eine Erklärung über Zweck und Art des Pflegedienstes, Maßnahmen zur Gewährleistung des Wohlbefindens und der Sicherheit der älteren Menschen, die ethischen Grundsätze, die angebotenen Dienste und Einrichtungen, das Management und das Personal in Bezug auf Fähigkeiten und Anzahl, Methoden zur Qualitätskontrolle und Beurteilung des Dienstes enthält.
- fordert den Anbieter auf, die Dienstleistungsbeschreibung mit dem Inhalt dieses Dokuments zu vergleichen und bietet bei Bedarf eine Erklärung, in der beschrieben wird, welche Abschnitte, Anforderungen und Empfehlungen, die nicht in der Dienstleistungsbeschreibung enthalten und daher nicht auf die Dienstleistungen des Anbieters anwendbar sind.
- kann vom Anbieter für interne Audits oder Selbstbeurteilung und/oder von externen Parteien für die Zertifizierung/Akkreditierung verwendet werden, um die Fähigkeit des Anbieters zu beurteilen, die Bedürfnisse und Erwartungen der älteren Person zu erfüllen.
- kann verwendet werden, um grundlegende Informationen für Beschaffung und Ausbildung zu geben.
- umfasst nicht die Normung von Medizinprodukten und klinischen Richtlinien.
Qualité des soins et de l'accompagnement des personnes âgées
Le présent document spécifie des exigences et des recommandations relatives à la fourniture de services de soins de santé et de services d’aide à l’autonomie pour les personnes âgées, dispensés par un personnel de santé ou un personnel de soutien à l’autonomie, que le service soit assuré au domicile des personnes ou dans une résidence médicalisée.
La fourniture du service est fondée sur les propres besoins et préférences de la personne âgée en vue de favoriser la liberté de choisir, la participation et une avancée en âge dans des conditions sécurisées.
Le présent document est applicable à tous les prestataires de services de soins et d’accompagnement des personnes âgées, quels que soient leur taille, leur structure, leur régime juridique ou leur mode de financement (public ou privé).
Le présent document ne couvre pas la normalisation des dispositifs médicaux et/ou des lignes directrices cliniques.
Kakovost oskrbe in pomoči za starejše
V tem dokumentu so določene storitve zdravstvene in socialne oskrbe za starejše, ki jih izvaja zdravstveno in socialno osebje. Ta dokument:
– določa zahteve in priporočila za storitve, ki se izvajajo za starejše v njihovem domačem okolju in domovih za ostarele na podlagi individualnih potreb oziroma preferenc glede samostojnega odločanja, sodelovanja ter varnosti v starosti;
– določa zahteve in priporočila za sistematične pristope v zvezi s sposobnostjo izvajalca storitev, da starejšemu zagotovi kakovostno oskrbo in podporo;
– zajema storitve ne glede na pravno obliko lastništva in ne glede na to, ali se storitev financira javno ali zasebno;
– se uporablja za izvajalce oskrbe, ne glede na strukturo, organizacijo, lastništvo, velikost ali vrsto storitev oskrbe;
– lahko izvajalec storitev uporablja na vseh ravneh upravljanja v organizaciji za načrtovanje, vodenje, izvajanje, vzdrževanje, vrednotenje in izboljšanje kakovosti storitve;
– lahko izvajalec uporablja za notranje presoje ali samoocenjevanje oziroma ga lahko uporabljajo tretje osebe za certificiranje/akreditacijo in tako ocenijo sposobnost izvajalca, da lahko zadovolji potrebe in pričakovanja starejšega;
– je mogoče uporabiti za zagotavljanje osnovnih informacij za namene preskrbe in izobraževanja;
– ne zajema standardizacije medicinskih pripomočkov in kliničnih smernic.
General Information
- Status
- Published
- Publication Date
- 30-Nov-2021
- Current Stage
- 9060 - Closure of 2 Year Review Enquiry - Review Enquiry
- Start Date
- 04-Jun-2025
- Completion Date
- 04-Jun-2025
Overview
CEN/TS 17500:2021 - "Quality of care and support for older persons" (CEN, Nov 2021) is a European Technical Specification that defines requirements and recommendations for health and social care services for older people. It covers services delivered at home and in care homes and promotes a person‑centred, rights‑based approach that supports autonomy, participation and safe ageing. The specification applies to providers of elder care regardless of ownership, funding, size or organizational model and explicitly excludes standardization of medical devices and clinical guidelines.
Key topics and requirements
CEN/TS 17500 structures quality of care around organizational processes and practical care domains. Key technical topics include:
- Organizational and management processes: governance, resources and systematic approaches to plan, lead, implement and improve care quality.
- Workforce competence: personnel knowledge, skills and staffing considerations to meet older persons’ needs.
- Ethical principles and rights: dignity, non‑discrimination, informed choice and participation.
- Integrated care and coordination: alignment of health and social care to avoid fragmentation and gaps in service.
- Health promotion and prevention: measures to maintain intrinsic capacity, nutrition, mobility and social wellbeing.
- Accessibility and built environment: adapting homes and care settings to support independence and inclusion.
- Assistive technology and related services: guidance on devices and systems that support daily living (excluding device standards).
- Infection prevention, hygiene and safety: cleaning, risk management and safe care practices.
- Assessment, documentation and care planning: initial needs assessment, agreements, care plans and ongoing review.
- Clinical and social care domains: cognition, mental health, medication management, palliative care, personal care, nutrition and activities.
- Quality assurance: continuous improvement, internal audits, self‑assessment, user feedback, complaints handling and evaluation.
Practical applications
CEN/TS 17500 is a practical tool for improving the quality of elder care and support:
- Use for service design and operational procedures in home care, assisted living and care homes.
- Use as a framework for internal audits, self‑assessment and preparation for external certification or accreditation.
- Inform procurement, staff training curricula and policy development.
- Support development of person‑centred care plans, integrated pathways and risk‑management systems.
Who should use it
- Care providers (public, private, non‑profit) delivering elder care at home or in residential settings
- Managers and clinical leads responsible for quality assurance and governance
- Procurement officers, educators and auditors involved in elder care services
- Policy makers and regulators designing age‑friendly services
Related standards
This Technical Specification complements broader standards and guidance on accessibility, quality management, infection control and integrated care frameworks. Refer to national standards bodies for implementation guidance and potential conversion into a European standard.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
CEN/TS 17500:2021 is a technical specification published by the European Committee for Standardization (CEN). Its full title is "Quality of care and support for older persons". This standard covers: The services specified in this document are health and social care services for older persons provided by healthcare and social care personnel. This document - specifies requirements and recommendations for services provided to the older person at home and in care homes, based on the older person's individual needs and preferences to assist self-determination, participation, and a safe and secure old age. - specifies requirements and recommendations for systematic approaches regarding the service provider’s ability to produce a good quality of care and support for the older person. - covers services irrespective of the legal form of ownership and whether the service is publicly or privately funded. - is applicable to care providers, regardless of structure, organization, ownership, size or type of the care services provided. - can be used by the service provider at all management levels in the organization to plan, lead, implement, maintain, evaluate and improve the quality of the service. - can be used by the provider for internal audits or self-assessment and/or external parties for certification/accreditation to assess the provider’s ability to meet the older person´s needs and expectations. - can be used to provide basic information for procurement and education. - does not cover standardization of medical devices and clinical guidelines.
The services specified in this document are health and social care services for older persons provided by healthcare and social care personnel. This document - specifies requirements and recommendations for services provided to the older person at home and in care homes, based on the older person's individual needs and preferences to assist self-determination, participation, and a safe and secure old age. - specifies requirements and recommendations for systematic approaches regarding the service provider’s ability to produce a good quality of care and support for the older person. - covers services irrespective of the legal form of ownership and whether the service is publicly or privately funded. - is applicable to care providers, regardless of structure, organization, ownership, size or type of the care services provided. - can be used by the service provider at all management levels in the organization to plan, lead, implement, maintain, evaluate and improve the quality of the service. - can be used by the provider for internal audits or self-assessment and/or external parties for certification/accreditation to assess the provider’s ability to meet the older person´s needs and expectations. - can be used to provide basic information for procurement and education. - does not cover standardization of medical devices and clinical guidelines.
CEN/TS 17500:2021 is classified under the following ICS (International Classification for Standards) categories: 11.020.10 - Health care services in general. The ICS classification helps identify the subject area and facilitates finding related standards.
CEN/TS 17500:2021 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
SLOVENSKI STANDARD
01-februar-2022
Kakovost oskrbe in pomoči za starejše
Quality of care and support for older persons
Qualität der Pflege älterer Menschen - Dienstleistungen, die in der eigenen Wohnung
erbracht werden, einschließlich betreutem Wohnen
Qualité des soins et de l'accompagnement des personnes âgées
Ta slovenski standard je istoveten z: CEN/TS 17500:2021
ICS:
03.120.99 Drugi standardi v zvezi s Other standards related to
kakovostjo quality
11.020.10 Zdravstvene storitve na Health care services in
splošno general
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.
CEN/TS 17500
TECHNICAL SPECIFICATION
SPÉCIFICATION TECHNIQUE
November 2021
TECHNISCHE SPEZIFIKATION
ICS 11.020.10
English Version
Quality of care and support for older persons
Qualité des soins et de l'accompagnement des Qualität der Pflege älterer Menschen -
personnes âgées Dienstleistungen, die in der eigenen Wohnung erbracht
werden, einschließlich betreutem Wohnen
This Technical Specification (CEN/TS) was approved by CEN on 17 October 2021 for provisional application.
The period of validity of this CEN/TS is limited initially to three years. After two years the members of CEN will be requested to
submit their comments, particularly on the question whether the CEN/TS can be converted into a European Standard.
CEN members are required to announce the existence of this CEN/TS in the same way as for an EN and to make the CEN/TS
available promptly at national level in an appropriate form. It is permissible to keep conflicting national standards in force (in
parallel to the CEN/TS) until the final decision about the possible conversion of the CEN/TS into an EN is reached.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia,
Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway,
Poland, Portugal, Republic of North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and
United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION
EUROPÄISCHES KOMITEE FÜR NORMUNG
CEN-CENELEC Management Centre: Rue de la Science 23, B-1040 Brussels
© 2021 CEN All rights of exploitation in any form and by any means reserved Ref. No. CEN/TS 17500:2021 E
worldwide for CEN national Members.
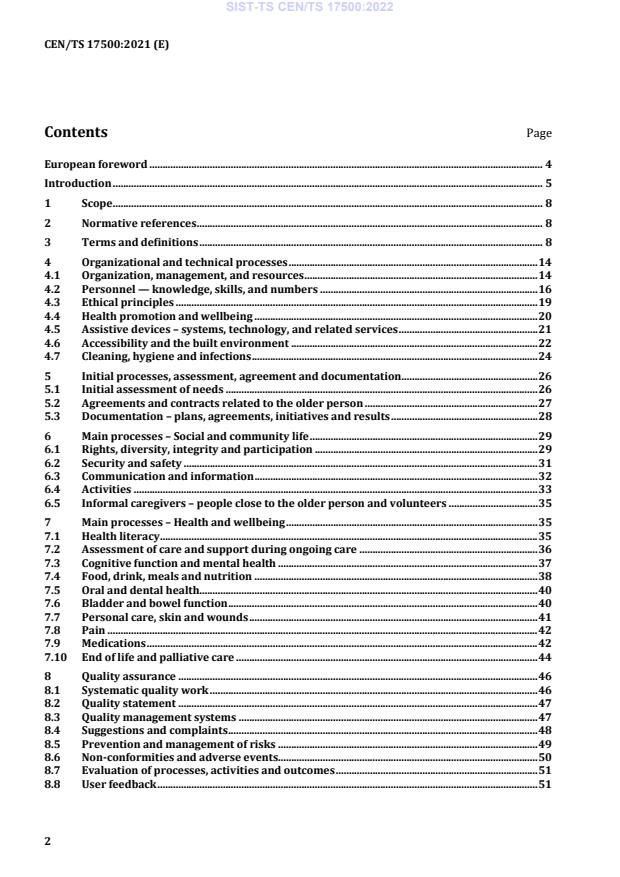
Contents Page
European foreword . 4
Introduction . 5
1 Scope . 8
2 Normative references . 8
3 Terms and definitions . 8
4 Organizational and technical processes . 14
4.1 Organization, management, and resources . 14
4.2 Personnel — knowledge, skills, and numbers . 16
4.3 Ethical principles . 19
4.4 Health promotion and wellbeing . 20
4.5 Assistive devices – systems, technology, and related services . 21
4.6 Accessibility and the built environment . 22
4.7 Cleaning, hygiene and infections . 24
5 Initial processes, assessment, agreement and documentation . 26
5.1 Initial assessment of needs . 26
5.2 Agreements and contracts related to the older person . 27
5.3 Documentation – plans, agreements, initiatives and results . 28
6 Main processes – Social and community life . 29
6.1 Rights, diversity, integrity and participation . 29
6.2 Security and safety . 31
6.3 Communication and information . 32
6.4 Activities . 33
6.5 Informal caregivers – people close to the older person and volunteers . 35
7 Main processes – Health and wellbeing . 35
7.1 Health literacy . 35
7.2 Assessment of care and support during ongoing care . 36
7.3 Cognitive function and mental health . 37
7.4 Food, drink, meals and nutrition . 38
7.5 Oral and dental health. 40
7.6 Bladder and bowel function . 40
7.7 Personal care, skin and wounds . 41
7.8 Pain . 42
7.9 Medications . 42
7.10 End of life and palliative care . 44
8 Quality assurance . 46
8.1 Systematic quality work . 46
8.2 Quality statement . 47
8.3 Quality management systems . 47
8.4 Suggestions and complaints . 48
8.5 Prevention and management of risks . 49
8.6 Non-conformities and adverse events . 50
8.7 Evaluation of processes, activities and outcomes . 51
8.8 User feedback . 51
8.9 Internal audits . 52
8.10 Self-assessment . 53
Annex A (informative) The integrated care concept, healthcare and social care . 54
Annex B (informative) Needs, wishes, assessment and assessment tools . 56
Annex C (informative) Compliance with requirements and recommendations . 60
Bibliography . 62
European foreword
This document (CEN/TS 17500:2021) has been prepared by Technical Committee CEN/TC 449 “Quality
of care for older people”, the secretariat of which is held by SIS.
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. CEN shall not be held responsible for identifying any or all such patent rights.
Any feedback and questions on this document should be directed to the users’ national standards body.
A complete listing of these bodies can be found on the CEN website.
According to the CEN/CENELEC Internal Regulations, the national standards organisations of the
following countries are bound to announce this Technical Specification: Austria, Belgium, Bulgaria,
Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland,
Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Republic of
North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and the
United Kingdom.
Introduction
Development of care and support
In Europe, the population of older persons requiring care and support services is increasing. Older
persons are generally defined according to a range of characteristics including chronological age,
change in social role and changes in functional abilities. In high-resourced countries older age is
generally defined in relation to retirement from paid employment and receipt of a pension.
There is a need for a shift in the way societies are organized and a change in the way older persons and
ageing in general are perceived. Building on the concepts of active ageing and age-friendly
environments, this document, Quality of care and support for older persons, stresses the importance of
enabling the older person in need of care and support to be involved and empowered to decide how
their needs, expectations and preferences can be met to live as autonomously as possible.
This document promotes the idea that the older person has the right to age with dignity, to be respected
and to be included as a full member of society. Promoting a rights-based approach means, for example,
fighting age discrimination, protecting service users’ rights, ensuring access to reliable and
comprehensive information, promoting a more accessible environment, and support for mobility,
communication, consultation, and participation.
Accessibility and availability of care and support services also play a critical role in ensuring the
inclusion of the older person. This means that the older person can use a service regardless of age,
geographical location, illness, disability, or functional limitation.
Important factors in quality development are that the older person maintains control over their own life
and that their needs and preferences are considered in the planning and provision of the care and
support. It should be a priority to develop a person-centred approach in all services, to maintain the
dignity, participation, and empowerment of the older person in need of care and support.
Provision of care and support needs to evolve
In general care and support of the older person services are of a good standard Despite this, threats to
the quality of care and support sometimes can come from outdated ideas and ways of working, which
often focus on keeping the older person alive rather than on supporting dignified living and maintaining
their intrinsic capacity. In this case, the older person may be regarded as a passive recipient of care and
support, and services may be organized around the service provider rather than the needs and
preferences of the older person. Care and support may focus on meeting the older person’s basic needs,
such as eating, showering or dressing, at the expense of the broader objectives of ensuring wellbeing,
that life has meaning, and that the older person feels respected.
With these aspects in mind, care and support ought to evolve in radical ways if the growing needs of
older persons are to be sustainably met. The transformation will require a coordinated and
multisectoral response that involves a wide range of stakeholders, both within and outside
governments. The most important participant being the provider, in the sense that it is the provider
who can ensure that the autonomy and will of the older persons are respected. More fundamentally,
mindsets about what care and support might comprise should be reset. New ways of thinking about
integrated care and support, and the systems for providing it, need to be developed. All relevant
stakeholders need to be responsive, empathetic, proactive, and innovative.
Changes need to encompass two broad areas. Firstly care and support of the older person needs to be a
priority agenda issue both societally and politically Second, care and support needs to be redefined.
Instead of thinking about care and support as a minimum and basic safety net that provides
rudimentary support to older persons who can no longer look after themselves, perceptions need to
shift towards a more positive and proactive agenda. Within this new framework, care and support
ought to be oriented towards both optimizing intrinsic capacity and compensating for a lack of capacity
to maintain the older person's integrity and functional ability and ensuring dignity and wellbeing and
the opportunity for activity and participation in society.
An integrated response ensures that the provision of care and support is optimized
In several European countries, the competencies for health services and social services are separated
from each other in two different service systems for older persons and is not considered as a specific or
separate sector of the social security system, and health and social services are not regulated by a single
legal scheme and administered by one single national and/or regional body. Thus, the healthcare and
the social care components of care are provided by different actors, which are registered, evaluated,
and operated according to different roles and organizational structures for healthcare and for social
care services. Depending on the degree of integration between healthcare and social care systems, the
care provided to the older person can be managed by one or several providers.
The integration between social care and health care, both administratively and at the points of use, is a
crucial factor in care quality. The separation of social care and health care services can result in
fragmented coverage, gaps in the provision of care and inappropriate use of acute services. More and
better coordination is needed at a systems level. See also Annex A (informative).
An integrated response to care and support covers very different types of care: health care, social care,
care for cognitive diseases, palliative and end-of-life care, services provided at home, in day care
centres, in day hospitals or in care homes, public or private-funded, informal care or care by volunteers.
Informal caregivers provide a high amount of care and support, for their beloved relative. The quality of
life of the informal caregiver is close linked to the quality of life of the older person in need of care and
support. Moreover, the provider can facilitate the building of networks with the aim of care providing
personnel giving support to the informal caregivers.
Health promotion and preventive approaches improve the quality of life of older persons
Health promotion and risk prevention offer the potential for improving the quality of life for the
growing population of older persons, while reducing the economic burden on the health system.
The World Health Organization describes health promotion as: ‘The process of enabling people to
increase control over, and to improve, their health.” It moves beyond a focus on individual behaviour
towards a wide range of social and environmental interventions.
A health promotion and prevention approach to care and support can provide the older person with the
knowledge and skills to remain independent and well for a longer period and to reduce the impact of
frailty syndromes e.g. falls, polypharmacy etc on their health and wellbeing Health promotion and
preventive approaches benefit not only the older person, but also the organizer and producer of care
and support services by reducing and postponing the need for heavy care and support services and thus
being cost-effective. Good and nutritious food, physical activity and strong social networks can help to
prevent illnesses and chronic diseases. Health consultation, counselling and safer treatment with
medication are other ways to prevent health risks among older persons.
How to read and apply this document
This document is intended to be useful to all types and sizes of providers in the private, public, and non-
profit sectors. While not all parts of this document will be of equal use to all types of providers, the
principles are relevant to every provider.
Provision of care and support consists of processes embedded in complex systems that are inevitably
linked to or require the incorporation of other existing and future standards outside of this document
and related to fields, such as accessibility (of processes, products, and services), ergonomics, social
responsibility, human resource management, assistive devices and products, sustainable development
in communities, smart homes, cognitive accessibility user interfaces, privacy and data management.
This document is an example of an interdisciplinary approach that has special focus on care and
support, and it is important that the provider identifies and incorporates the use of other
complementary standards.
This document uses the term ‘care and support’ for the combination of healthcare services and social
care services. The document aims to facilitate the development of care and support services by
establishing common denominators that are agreed on as fundamentals of care and support.
This document can be used by the service provider at all management levels in the organization to plan,
lead, implement, maintain, evaluate, and improve the quality of the service.
When starting to use this document, each service provider
— describes the organizations service content in a service description, which includes for example a
statement of purpose and character of the care and support service, measures for ensuring the
older persons’ wellbeing and security, the ethical principles, the services and facilities provided,
management and personnel in terms of skills and numbers, methods for quality control and
evaluation of the service.
— compares the service description with the content of this document and, when needed, gives a
statement that lists what clauses, requirements and recommendations that are not in the service
description and therefore not applicable to the provider’s services.
The document can be used by the provider for internal audits or self-assessment and/or external
parties for certification/accreditation to assess the provider’s ability to meet the older person’s needs
and expectations.
The document can be used to provide basic information for procurement and education of the
personnel.
Establishing quality of care and support for older persons requires knowledge of the ageing process, a
gerontological skill set and a positive attitude to ageing. . Involvement and engagement of all
management chain is crucial when implementing quality of care and support for older persons. When
the management is committed to quality requirements and recommendations, they pass down
knowledge to their personnel and motivate them to be involved. Good communication helps to create a
committed and supportive atmosphere, and thus has a positive influence on the implementation of this
document and continuous improvement of quality.
The requirements and recommendations given in this document are actions to be taken by the provider.
Requirements and recommendations are listed in Clauses 4 to 8 after the introduction and explanation
of the terminology used. These sections start with short general introductions which provide a brief
background to the following requirements and recommendations.
This document uses the words ‘general’ and ‘specific’ in relation to requirements and recommendations
in the following way:
• General requirements and general recommendations apply to all care and support services
regardless of whether they are provided at home or at a care home.
• Specific requirements and specific recommendations apply mainly to care and support services
provided in a care home but shall/should also be applied to care and support services given at
home when such services are in the service description of the provider.
1 Scope
This document specifies requirements and recommendations for the provision of health and social care
services for older persons provided by healthcare and social care personnel, irrespective of whether the
service is provided in the persons own home or in a care home.
Service provision is based on the individual needs and preferences of the older person to assist self-
determination, participation and a safe and secure old age.
This document applies to all providers of care and support to older persons irrespective of size,
structure, legal set up, or funding model (i.e. public or private).
This document does not cover standardization of clinical guidelines and/or medical devices.
2 Normative references
There are no normative references in this document.
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— IEC Electropedia: available at https://www.electropedia.org/
— ISO Online browsing platform: available at https://www.iso.org/obp
3.1
care and support
activities within health care services, social care services or an integration of both, including care
provided by informal carers
Note 1 to entry: An informal carer includes any person such as a family member, friend, or a neighbour, who
provides regular ongoing assistance to another person.
Note 2 to entry: Support is mixture of practical, financial, social, and emotional activities for persons who need
extra help to manage their lives and to be independent.
[SOURCE: EN 17398:2020 modified. Support introduced in title and Note 2 added]
3.2
service
output of a provider with at least one activity necessarily performed between the provider and the
customer
Note 1 to entry: The dominant elements of a service are generally intangible.
Note 2 to entry: Service often involves activities at the interface with the customer to establish customer
requirements as well as upon delivery of the service and can involve a continuing relationship such as banks,
accountancies, or public organizations, e.g. schools or hospitals.
Note 3 to entry: A service is generally experienced by the customer.
[SOURCE: ISO 9000:2015, 3.7.7 modified — definition has been abbreviated and aligned with 3.24]
3.3
healthcare services
services covering the whole spectrum of care, from promotion and prevention to diagnostic,
rehabilitation and palliative care, as well as all levels of care including self-care, home care, community
care, primary care, long-term care and hospital care for the purpose of providing integrated health
services throughout life
[SOURCE: EN 17398:2020]
3.4
social care services
activities undertaken by social care personnel that focus on help and support in coping with activities of
everyday life
Note 1 to entry: The content of the social care varies between the European countries and in some countries,
health and social care are integrated and the tasks carried out in the elderly care can thus not be divided into
healthcare or social care.
Note 2 to entry: Social care also aims to prevent abuse and neglect.
3.5
integrated care
coordinated provision of care and support (public, private, personal/family/informal) provided to
ensure practicable autonomy and independence of the older person
3.6
care provider
organization or care professional providing care and support services to older persons in need of care
and support
Note 1 to entry: Depending on the needs of the older person the care and support can be provided at the persons
own home, day care centres or care homes.
Note 2 to entry: The service can be provided by public, private or non-profit organizations.
Note 3 to entry: The service can consist of healthcare, social care, or a combination of both.
3.7
care home
place of residence for persons with physical and/or mental disabilities, who may require nursing care
to perform daily living activities
Note 1 to entry: The facility provides 24-h supervision, nursing care, rehabilitation programmes and social
activities as well as assisting contact with the social environment, including assistance with asserting rights,
justified interests, and handling personal matters.
Note 2 to entry: care homes are often referred to as nursing homes.
Note 3 to entry: A care home might specialize in certain types of disability or conditions such as dementia.
3.8
home
habitual residence, such as an apartment or house, of the older person and their family
Note 1 to entry: The older person’s home can be located in an accommodation specifically designed for older
persons
3.9
home care
healthcare and social care given at the person's home aimed at preserving and increasing functional
ability and enable the older person to remain at home
Note 1 to entry: The care and support is provided to older persons in their own homes with a view to not only
contributing to their life quality and functional health status, but also to replace hospital care with care in the
home for societal reasons. Home care can cover a wide range of activities, from preventive visits to end-of-life
care.
3.10
individual care plan
plan developed on the basis of initial and continuous assessment of needs, expectations, objectives and
individual resources developed by the care team (including plans developed by professionals, see 3.22)
of the provider or by the commissioner of the care in cooperation and agreement with the older person
Note 1 to entry: The older person’s individual care plan covers all aspects of health and social care and describes
how these will be met in terms of daily living and longer-term outcomes. The plan also includes plans for how and
when evaluations and reassessments are carried out.
Note 2 to entry: In many European countries, plans and records concerning healthcare and social care are kept as
separate entities and governed by different laws. When that is the case, it might not be possible to include both
healthcare and social care in one plan. In cases of separate healthcare and social care plans, it is necessary to
convey information to providers and members of personnel to the extent permitted.
Note 3 to entry: There are differences in the legislation governing care services the European countries. With
respect to the care and support that the society is responsible for providing, the individual care plan sometimes
must be implemented in conjunction with an administrative decision or approval.
3.11
care personnel
personnel involved in the direct provision of care and support services
[SOURCE: EN 15224:2012, 3.6.2 modified, the word “health” has been deleted in title]
3.12
care professional
personnel with a professional entitlement in a given jurisdiction involved in the provision of care and
support services
Note 1 to entry: Professional entitlement in a given jurisdiction, (formally regulated field), describes requirements
issued by a competent authority to be fulfilled in order to be qualified by formal, official, or legal certification,
registration or authentication to perform for example legal decisions, diagnosis, therapy or treatment.
[SOURCE: EN 15224:2012, 3.6.3 modified, the word, “health” has been deleted in title and “involved in
the provision of care services” and a Note to entry has been added.]
3.13
policy
document specifying the intentions and direction of an organization as formally expressed by its top
management
Note 1 to entry: This constitutes one of the common terms and core definitions for ISO management system
standards given in Annex SL of the Consolidated ISO Supplement to the ISO/IEC Directives, Part 1.
[SOURCE: EN ISO 9000:2015, 3.5.8, modified, “document specifying” added]
3.14
procedure
specified way to carry out an activity or a process
Note 1 to entry: Procedures can be documented or not.
[SOURCE: EN ISO 9000:2015, 3.4.5]
3.15
health
state of complete physical, mental, and social wellbeing and not merely the absence of disease or
infirmity
Note 1 to entry: Health has many dimensions (anatomical, physiological, and mental) and is largely culturally
defined.
Note 2 to entry: Definition refers to ‘good’ health.
[SOURCE: WHO Ageing and Health Technical Report, Vol.5[4], modified — Note 2 to entry has been
added]
3.16
frailty
extreme vulnerability to endogenous (e.g. biological ageing) and exogenous (e.g. diseases or
pharmacological treatment) stressors that exposes an individual to a higher risk of negative health-
related outcomes
Note 1 to entry: Frailty also exposes an individual to a higher risk of negative social outcomes.
[SOURCE: WHO. World report on ageing and health. 2015, modified]
3.17
person-centred care
an approach in which patients take part in their care, self-care and in the decision-making process
[SOURCE: EN 17398:2020]
3.18
abuse
single or repeated act or lack of appropriate action which causes harm or distress to an older person or
violates human and civil rights
Note 1 to entry: Abuse may include physical abuse, psychological abuse, sexual abuse, financial exploitation, and
neglect. Elder abuse may occur in different situations, including at home within the family, at home in connection
with the provision of services or at a care home. It can be intentional or unintentional.
[SOURCE: WeDO: Wellbeing and Dignity of Older people, 2012]
3.19
restraint
intentional restriction of a person’s voluntary movement or behaviour
Note 1 to entry: Physical restraint is any manual method, or physical or mechanical device, material or equipment
attached or adjacent to the person’s body that the individual cannot easily remove, and which restricts freedom of
movement or normal access to one’s body.
Note 2 to entry: Chemical restraint is the intentional use of medication to control or modify a person’s behaviour
or to ensure a person is compliant or not capable of resistance, when no medically identified condition is being
treated or where the treatment is not necessary for the condition.
Note 3 to entry: Environmental restraint is the intentional restriction of a person’s normal access to their
environment, with the intention of stopping them from leaving or denying a person their normal means of
independent mobility.
[SOURCE: Ireland Department of Health. Toward a Restraint Free Environment in Nursing Homes,
2011, abbreviated]
3.20
medication review
formal review process performed at specified intervals or when relevant, in which healthcare personnel
and the older person collaborate to ensure correct and adequate medical prescriptions and transfer of
information at every transition from one care provider to another
Note 1 to entry: The medication review is a systematic process for obtaining a medication prescription history and
using that information to compare medication prescriptions in order to identify and resolve discrepancies and to
prevent potential medication errors and adverse effects of medicinal products.
3.21
palliative care
approach that improves the quality of life of patients and their families when facing problems
associated with a life-threatening illness, through prevention and relief of suffering
Note 1 to entry: Palliative care includes symptom management during both acute and chronic illness and end-of-
life (terminal) care by means of early identification, assessment and treatment of pain and other problems,
physical, psychosocial, and spiritual.
[SOURCE: WHO: https://www.who.int/cancer/palliative/definition/en/]
3.22
clinical guideline
set of systematically developed statements to assist the decisions made by healthcare actors about
healthcare activities to be performed with regard to specified health issues
[SOURCE: EN ISO 13940:2016, 9.2.4]
3.23
record
document stating results achieved or providing evidence of activities performed
Note 1 to entry: It can be, for example, medical records from physicians, nursing records from registered nurses or
social documentation from certified assistant nurses or record from social care services.
[SOURCE: EN ISO 9000:2015, modified, a Note to entry has been added]
3.24
accessibility
extent to which products, systems, services, environments, and facilities can be used by people from a
population with the widest range of characteristics and capabilities to achieve a specified goal in a
specified context of use
Note 1 to entry: Context of use includes direct use or use supported by assistive technologies.
Note 2 to entry: Adapted from ISO/TR 22411:2008, definition 3.6.
[SOURCE: ISO 26800:2011, 2.1]
3.25
adverse event
unintended event that has a negative influence upon healthcare processes
Note 1 to entry: In the European Vigilance System, an adverse event is described as: Any untoward medical or
nonmedical event or occurrence, unintended disease or injury or any untoward clinical signs including abnormal
laboratory findings in subjects of care during or shortly after treatment, whether related or not related to the
treatment.
[SOURCE: EN ISO 13940:2016]
3.26
telehealth service
healthcare activity supported at a distance by information and communication technology services
[SOURCE ISO DIS 13131:2021]
3.27
volunteering
person or activity of doing something without enumeration, for the benefit of the older person or their
care environment
Note 1 to entry: volunteering is a freely made choice by the individual that may or may not be a relative.
3.28
whistleblowing
reporting of a wrongdoing within an organization
Note 1 to entry: The reported concern must be a genuine concern about a crime, criminal offence, miscarriage of
justice, dangers to health and safety and the environment, understaffing, missed care (care left undone), dignity,
self-determination, neglect, abuse and violence/either of the older person or personnel and the cover up of any of
these.
Note 2 to entry: Some EU countries do not allow anonymous whistleblowing.
[SOURCE: The Whistleblowing Helpline. UK, modified]
4 Organizational and technical processes
4.1 Organization, management, and resources
4.1.1 General
Important factors for the creation of a good, safe and secure care and support service for the older
person are the resources, particularly: the organizational structure, distribution of responsibilities, a
good and safe working environment, terms of employment, personnel – quantity and competence,
economy, including financial support by the government or private institutions, facilities, premises,
infrastructure, assistive devices and technology and the ethical principles that underpin it.
The organization provides the care and support in compliance with, for example, authorization,
contract, or procurement agreement to ensure that the needs of the older person are met.
Good practice regarding promotion and marketing might refer to robust, validated and openly available
research and/or evaluations that specifically relate to the service.
Efficient leadership and management in the use of available resources is fundamental to provide a
person-centred, safe, and effective care and support service that meets the needs of the older person
and to respect their dignity and wishes. A well-run care and support service uses resources effectively
and seeks opportunities to provide a sustainable and continuously improved service, which achieves
optimum outcomes for the older person. Resource decisions take in account the views and needs of the
older person.
The main purpose of decisions and actions taken at other levels of the organization should be aimed at
enabling the frontline personnel to provide a good, safe, and secure care and support service.
The conditions for high quality, person-centred care is an organization that is flexible and operates in
multi-professional teams that involve the older person.
Written policies and procedures give guidance to personnel and promote consistency in application. To
accomplish this consistency, policies and procedures are documented in enough detail and
communicated in a structured way to enable personnel to carry out the care and support activities in a
safe and consistent manner.
4.1.2 Organization, management, and resources — General requirements
The provider of the services shall:
a. ensure that the organization has systems to identify, implement and ensure compliance with all
relevant and applicable legislation concerning planning, implementation, evaluation, and follow-up
of the service.
b. define the organizational structure and clearly describe the powers and responsibilities of
individual roles.
c. ensure that policies and procedures concerning health care are based on clinical guidelines and
existing recommendations established by competent authorities, organizations and medical
societies.
d. ensure that there is a publicly available and accessible statement of purpose for the care and
support service that clearly describes the model of care and support including the older persons’
wellbeing and safety, ethical framework, the services and facilities provided, management and
personnel in terms of knowledge, skills and numbers.
e. ensure that the responsibility for the quality of care and support is clearly addressed in contracts
and agreements between the provider and other providers, sub-contractors and care professionals.
f. have written policies and procedures that includes but are not limited to care and support, social
environment, physical environment, facilities, devices, safety and security, personnel and
administration:
1. to ensure that the use of available resources is planned and managed to provide person-
centred, effective, and safe care and support to the older person.
2. to clarify and facilitate the coordination of care and support between the provider and other
providers, sub- contractors, and care professionals.
3. to ensure that governing/guiding documents for the care and support service set clear
objectives for the provision of person-centred, safe, and effective services with a focus on
improved outcomes for the older person.
4. to ensure that personnel’s terms of employment (e.g. collective agreements and enterprise-
based agreements) are described and available.
5. to ensure a good working environment and occupational safety and health of personnel so that
they can fulfil their care and support tasks effectively, safely and with good quality.
g. ensure that policies and procedures are communicated and accessible to personnel and for relevant
stakeholders and authorities.
h. ensure that personnel receive the necessary information and training to enable effective
implementation of policies and procedures.
i. have a system for the development and maintenance of policies and procedures and ensure that
they are reviewed at regular intervals.
4.1.3 Organization, management, and resources — General recommendations
The provider of the services should:
a. ensure that policies and procedures are drawn up in consultation and collaboration with personnel
when relevant.
b. ensure that claims regarding the health and social care credentials of the service and its personnel,
the technologies used and claims regarding service outcomes are clearly described, appropriately
evidenced and comprehensible by the older person.
c. offer the older person guidance and information to other providers/professionals if the service
provider lacks available resources that corresponds to the needs of the older person.
d. ensure that sustainability measures are incorporated into the planning, management and use of
resources.
4.2 Personnel — knowledge, skills, and numbers
4.2.1 General
Personnel numbers, their knowledge, skills, and attitudes together with competent and available front-
line management are close linked with the quality and effectiveness of the care and support. These
factors are important and have a decisive influence on the possibility for the older person to get the care
and support indicated by the assessed service needs.
Providing care and support services for older persons can be complex and challenging for the
personnel. All personnel working with older people must have a level
...



Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...